Plato said what has become one of the most memorable quotes in modern history, “Necessity is the mother of all invention”. That statement is most certainly true for Africa’s healthcare. Research by the World Bank indicates that Sub-Saharan Africa, on average, has the worst healthcare in the world. It accounts for a quarter of all disability and death caused by disease worldwide, yet has only 1% of global health expenditure and just 3% of the world’s health workers.
Infrastructure is poor as a result of inadequate investment in the healthcare industry. This reality makes even the most basic medical care difficult.
However, it is this reality that has created a necessity that has resulted in the emergence of new technologies – from drones to apps to AI and blockchain-powered virtual assistants. The rise of new technologies is helping break down these barriers and provide vital medicines to many more people.
The rise in the use of technological innovations in Africa’s healthcare has been primarily one of survival. From addressing the shortage of healthcare workers, to driving innovation, pruning systems of vested interests and discarding moribund western systems – the continent has not much of a choice but to piggyback on technology.
Using technology to leapfrog to the future.
Experts have argued that by 2030, the global demand for health workers will rise to 80 million, double the current number while the supply may not cross 65 million. This adversely affects low-income countries seeking to achieve adequate growth in both the demand and supply of expertise necessary to cover basic health services.
This is a serious problem as some countries like Ghana, Senegal, South Africa and Zimbabwe are already having an exodus of healthcare workers leaving for the UK, and Canada. Health clinics in Zimbabwe are facing a crisis as an increasing number of doctors and nurses leave the country in search of better prospects. Faced with this reality governments have only a few tricks up their sleeves to circumvent the crisis. The only plausible solution is to innovate and to do so even faster.
AI and blockchain
In recent years Africa has seen a growing number of startups building healthcare innovations that have proven to have so much potential. African governments have also made tremendous strides in supporting healthtech innovations in the last few years and this trend is only growing ever since the outbreak of the COVID-19 pandemic a couple of years back.
The COVID-19 pandemic has galvanised the development of more than 120 health technology innovations that have been piloted or adopted in Africa, a World Health Organisation (WHO) analysis found.
The study of 1000 new or modifications of existing technologies that have been developed worldwide to target different areas of the COVID-19 response found that Africa accounts for 12.8% of the innovations. The response areas include surveillance, contact tracing, community engagement, treatment, laboratory systems and infection, prevention and control.
In Africa, 57.8% of the technologies were ICT-driven, 25% were based on 3D printing and 10.9% were robotics. The ICT-based innovations include WhatsApp Chatbots in South Africa, self-diagnostic tools in Angola, contact tracing apps in Ghana and mobile health information tools in Nigeria. The countries with the most innovations were South Africa (13%), Kenya (10%), Nigeria (8%) and Rwanda (6%).
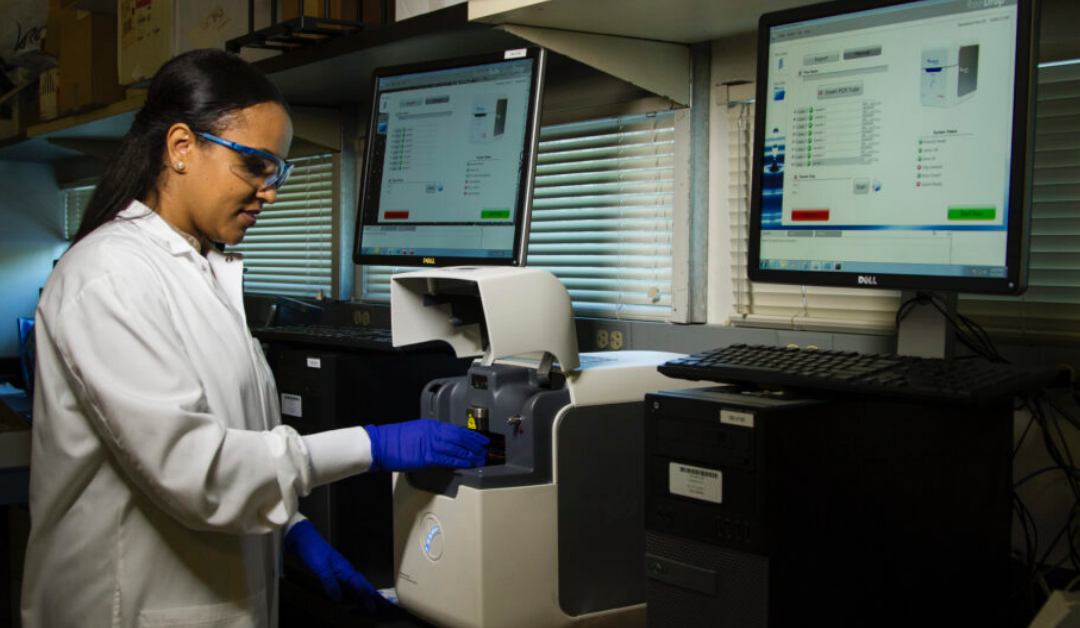
New technologies such as Artificial Intelligence (AI) and Blockchain are being used in varying ways to tackle problems in the healthcare industry. Kenyan startup Neural Labs is using AI-enabled medical imaging to facilitate real-time diagnosis of various respiratory, heart and breast diseases and pathologies.
Founded in January 2021 by Tom Kinyanjui and Paul Mwaura Ndirangu, two machine learning engineers, Neural Labs has developed a platform called NeuralSight in a bid to reduce Africa’s disease burden and hospital workloads, with better patient outcomes and democratised access to healthcare.
NeuralSight can identify, label and highlight over 20 respiratory, heart and breast diseases and pathologies, including pneumonia, tuberculosis, COVID-19, emphysema, and more. The co-founders have been working on different AI-focused technologies since 2020, eventually zeroing in on tackling healthcare challenges.
Another Kenyan-founded startup, Ilara Health provides accessible and affordable diagnostics to the disadvantaged who are reportedly up to 500 million people in Africa.
The startup partners with companies using artificial intelligence and robotics to lower the overall cost of diagnostics and integrate these companies’ devices onto its platform. Ilara Health procures tech-powered diagnostic equipment at affordable prices and makes the same equipment available to healthcare facilities then pay over some time.
Nigeria’s Healthtracka allows users to book health screening tests from the comfort of their homes and get test results delivered within 1-3 days via email. The health tests offered include a COVID-19 PCR test, a sexually transmitted disease test, and a full body checkup. All test results are reviewed and confirmed accurate by medical professionals before they are released.
The startup joined the Techstars Toronto Accelerator programme in 2021 barely five months after launch. Last December, it also partnered with Fleri Inc., a United States-based insurtech startup enabling immigrants to provide healthcare for their loved ones back home.
Here in Zimbabwe, the government parastatal POTRAZ has been sponsoring and funding startups that have the potential to have an impact, mostly the ones in healthtech. The first year of the innovation drive was targeted towards startups that were working on solutions to curb the spread and or treat the COVID-19 virus. Startups that were building cheaper respirators and building apps for COVID-19 contact tracing were selected for funding.
Not to be left out by any chance, as a co-founder of a little-known startup QuStack, we were one of the selected startups at this year’s hackathon to get funding. The solution we are building uses AI and Natural Language Understanding (NLU), the goal is to address some key of our health system, amongst them being providing relevant medical information through social networks like WhatsApp and connecting patients to doctors in real-time bonus of the solution is optimising the pharmaceutical value chain by ensuring people can buy medication, both over-the-counter and prescriptions through their favourite social network.
AI’s capabilities make it useful in the detection of disease. It can detect lung cancer and provide a diagnosis comparable to a CT scan, thus, making it an important tool in the healthcare arsenal.
Drones
As an African, I am pleased that Rwanda was the first nation in the world to use drones to deliver blood and essential medicines to rural hospitals. This extraordinary feat came following an agreement between the government and US manufacturer Zipline, and two centres now operate in the east and west of the country.
Since 2011, Zipline has been working with the government of Rwanda to deliver blood supplies to about 21 regional hospitals — launching more than 50 drones daily for on-demand deliveries. The company is planning to soon deliver vaccines and medicines to hundreds of clinics in Rwanda, and also in Tanzania.
“The lack of paved road infrastructure in these countries makes running a road-based delivery network difficult,” said Keenan Wyrobek, co-founder and head of product and engineering at Zipline. “There’s nothing worse than a doctor who can’t help a patient simply because of a lack of supplies.” Again, necessity proves to be the mother of innovation.
Before Zipline, blood would often expire on the shelf in Rwanda. Doctors can request blood on demand, by calling or placing orders online, and it generally arrives within 30 minutes. The drones gauge wind speed and direction when releasing a package, with its parachute, so that it falls in a dedicated area. Round trips are 150 kilometres or less, and each drone makes a single drop before returning to the distribution centre. One of the biggest challenges has been navigating deliveries through mountain passes or during storms.
Other African countries are following suit on what Rwanda has proved to be possible. Uganda is delivering HIV medicine by drone in an archipelago in Lake Victoria, a pilot programme aiming to improve the transport of medical supplies for the country’s health system, which faces chronic shortages.
The trial is funded by the pharmaceutical giant Johnson & Johnson and operated by the government-run Infectious Diseases Institute. It delivers HIV drugs from a hospital to patients in rural hamlets in Kalangala.
Malawi is using low-cost drones to deliver medicines. Students built the EcoSoar drone for remote medicine delivery and remote sensing purposes. Quite a nice play on the name, EcoSoar. This aviation milestone was achieved as a team from Virginia Tech supervised a fully autonomous, 19 km simulated drug delivery flight in a drone designed at Virginia Tech and built by Malawian students.
Technology has proven very useful in Africa’s healthcare and seeing its use alleviates the plethora of problems that exist in the industry. Millions of Africans do not have their medical records digitized as the government-funded and run hospitals and clinics still stifle the advancement of technology. Thousands of qualified healthcare workers are still leaving the continent for greener pastures in Europe and North America.
As we get accustomed to this reality of modernity, African policymakers will need to architect modern privacy frameworks to ensure patients’ rights would be respected and rightfully safeguarded against any potential abuses. The technology will only work to the extent that governments across African communities work proactively to ensure smart policies.